Discover why insurance claims still take 30 days and how AI agents cut cycle times to real-time, reducing costs and boosting satisfaction.


.png)
Claims are the moment of truth in insurance. They’re when policyholders discover if their insurer can truly deliver on its promise. Yet for decades, this moment has been defined by long waits, endless paperwork, and growing frustration. According to J.D. Power, nearly a third of customers report dissatisfaction with their claims experience, and settlement speed is the number one reason (J.D. Power, 2023 U.S. Auto Claims Satisfaction Study). McKinsey adds that close to 60% of customers who leave their insurer do so because claims resolution simply takes too long (McKinsey).
The problem isn’t mysterious. Most insurers are still saddled with manual review, siloed systems, and outdated compliance checks. Even with digitization, the average claim still takes three to six weeks from filing to payout (BBJ Lawyers).
Breaking Down the Traditional Claims Workflow

Figure 1: The traditional insurance claims workflow — from FNOL to payment — is filled with manual handoffs and bottlenecks that stretch processing into weeks. Image Source: Wondershare EdrawMax
The process itself hasn’t fundamentally changed in decades: a policyholder reports a loss, the claim is validated against coverage, adjusters investigate, and finally payment is issued. At each stage, friction creeps in.
Intake data often arrives incomplete or inaccurate, triggering back-and-forth requests. Adjusters spend over an hour per claim on manual data entry and validation (Inovalon). Outdated systems mean the same information gets keyed into multiple platforms, and regulatory reviews add further delays.
It’s no surprise that many policyholders end up calling multiple times for updates — and J.D. Power reports that those who call more than twice are 80% more likely to switch carriers.
How AI Agents Change the Game

Figure 2: AI agents streamline the claims journey by automating intake, triage, and fraud detection, reducing settlement time from weeks to minutes. Image Source: vlinkinfo.com
This is where AI agents enter the picture. Unlike traditional automation tools that require endless rule-writing, AI systems are designed to learn, adapt, and execute across the entire claims journey.
Take intake and validation. With natural language processing (NLP), AI can pull structured data directly from unstructured forms, emails, and attachments. That means policy details, loss dates, and eligibility checks happen instantly, without human retyping. In the Nordic region, one insurer used AI-powered document intelligence to cut processing from weeks to minutes (Vlink Info).
Or consider triage. AI models can analyze millions of claims to predict which ones are straightforward and which ones carry hidden risks. Routine auto damage can be fast-tracked, while a complex medical claim gets routed to a human adjuster. Tools like CLARA Triage even learn from adjuster feedback to continuously improve routing accuracy (CLARA Analytics).
Fraud detection may be the most dramatic example. Fraud costs U.S. insurers an estimated $308.6 billion annually (Coalition Against Insurance Fraud). Traditional rule-based systems miss too much. AI, by contrast, can flag suspicious patterns in behavior, documents, or even images — catching fraud rings that previously went unnoticed (Salesforce).
The Technology Behind It
Three technologies are driving this shift:
- Optical Character Recognition (OCR): Turns scanned or handwritten documents into structured, machine-readable data — with some systems now processing hundreds of pages in seconds (BaseCap Analytics).
- Natural Language Processing (NLP): Goes beyond keywords to actually understand context, filling in missing details and reducing human error (Shepherd Insurance).
- Generative AI: Summarizes claims into concise reports, highlights red flags, and provides adjusters with faster recommendations (Arize AI).
Individually, these tools improve efficiency. Together, they make real-time claims processing a reality.
From Concept to Execution
Of course, this transformation doesn’t happen overnight. Insurers that succeed follow a clear roadmap:
First, they train models on insurance-specific data rather than generic public datasets, reducing bias and boosting accuracy (Kili Technology). They then start fast by leveraging pre-trained AI processors, like Google Cloud’s Document AI, which helped Loadsure reach 95% extraction confidence almost immediately (Google Cloud). And finally, they measure progress rigorously — not just in “accuracy,” but in F1 scores, drift, and cycle time reduction (Arize AI).
The message is simple: don’t wait to build the perfect system. Start small, measure, and scale.
Measuring Success: From 30 Days to Real-Time
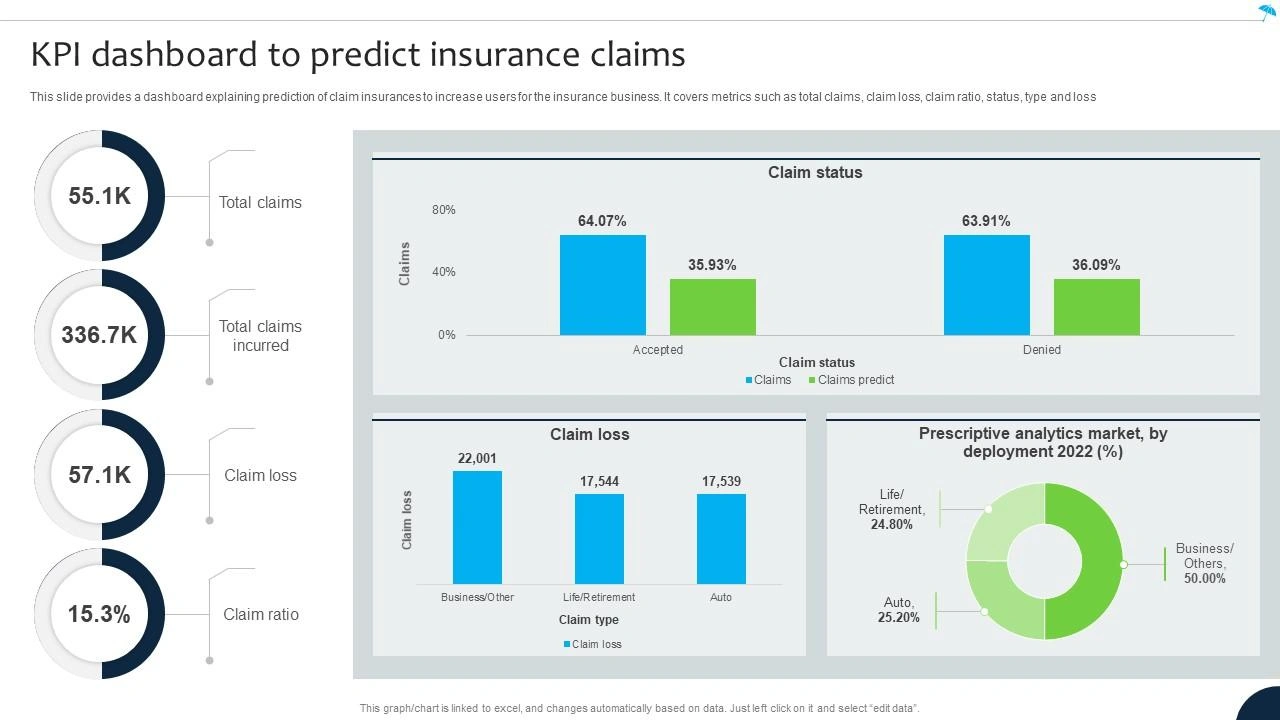
Figure 3: With OCR, NLP, and Generative AI working together, insurers are seeing >95% accuracy in production and cycle times reduced from 30 days to under 1 day. Image Source: SlideTeam
The results speak for themselves. A leading travel insurer processing 400,000 annual claims cut its cycle from three weeks to minutes (Salesforce). Document intelligence tools now achieve extraction accuracies above 95%, in some cases approaching 99.9% (Google Cloud). And customer satisfaction rises when claims become transparent, accurate, and — above all — fast.
What You Should Do Next
If there’s one lesson here, it’s this: 30-day claims cycles aren’t just inefficient — they’re a competitive liability.
Insurers can and should start acting now. Benchmark your claims process against industry standards. Identify the bottlenecks where automation will have the most impact. Launch a pilot project to prove the value. Early adopters are already seeing faster settlements, lower costs, and stronger customer loyalty.
Conclusion: From 30 Days to Real-Time
The insurance industry has reached a turning point. Customers no longer accept 30-day delays, and competitors who embrace AI agents are already cutting cycle times to hours — sometimes minutes. OCR, NLP, and Generative AI aren’t future technologies; they’re in production today, delivering 95%+ accuracy, lower costs, and higher satisfaction.
The message is clear: insurers that modernize now will build trust, protect margins, and win market share. Those that wait will be left behind.
Don’t let 30 days define your claims process. See How AI Can Cut Your Claims Cycle
FAQs
Q1. How does AI transform the insurance claims process?
AI doesn’t just automate individual steps — it connects the entire claims lifecycle. OCR converts paper and scanned files into structured data. NLP validates policy details and extracts meaning from adjuster notes or unstructured forms. Generative AI summarizes key findings and even fills in missing details. Together, these tools cut processing time from weeks to minutes while reducing errors and manual rework.
Q2. What slows down traditional claims processing?
Legacy claims workflows are full of friction:
- Manual data entry wastes ~70 minutes per claim.
- Incomplete information often leads to denials or back-and-forth requests.
- Siloed systems require the same data to be entered multiple times.
- Compliance checks are manual and inconsistent.
All of this extends average settlement times to 30 days or longer, frustrating both insurers and policyholders.
Q3. How accurate are AI-powered claims systems?
Modern AI claims platforms regularly deliver 95–99% extraction accuracy. In production environments, some reach 99.9% “clean claim” rates, meaning they process without manual intervention. This isn’t just theoretical — insurers using tools like Google Cloud Document AI or advanced OCR report faster, more accurate outcomes than experienced human adjusters.
Q4. How does AI affect customer satisfaction?
Customer satisfaction is directly tied to speed and transparency. J.D. Power found that customers who had to call more than twice about their claim were 80% more likely to switch providers. With AI, claims can be settled in hours instead of weeks, giving customers faster payouts, real-time status updates, and confidence in the process. That trust translates into higher retention and stronger Net Promoter Scores (NPS).
Q5. What’s required for a successful AI rollout in claims?
Success isn’t about buying a tool — it’s about strategy. Insurers need:
- Domain-specific data: Models trained on insurance datasets avoid bias and improve accuracy.
- Pre-trained processors: These accelerate deployment while maintaining confidence scores above 95%.
- Performance monitoring: Tracking F1 scores, drift, and error rates ensures the system improves over time.
- Change management: Staff should be trained to work alongside AI, using it as a co-pilot rather than a replacement.
Browse Similar Articles
Accelerate Your Agent Roadmap
Adopt gives you the complete infrastructure layer to build, test, deploy and monitor your app’s agents — all in one platform.




.svg)
.svg)